The Discovery of Factor X
Blood clotting issues have been a great concern for people for many centuries. The disease known as scurvy has plagued sailors that endured spans of time at sea without eating vegetables and citrus fruit causing severe bleeding. The British Navy insisted that its vessels stock vegetables and citrus fruit since the 18th century. Since that time a significant amount of knowledge has been gained and discoveries made regarding this critical area of research.
All the way back in 1904 Dr. Morawitz hypothesized that prothrombin converted into thrombin in the presence of calcium and thromboplastin and that fibrinogen converted into fibrin in the presence of thrombin, which finally caused blood to clot.
During the first half of the 20th century, there were a plethora of blood clotting factors were discovered. At the midpoint of the 20th century, between the years 1947 to 1952, there were annual conferences known as the Macy conferences on Blood Clotting. This was a prolific time for the field of research and a nomenclature needed to be created to remove the confusion from clinicians discovering the same factors in different labs and giving them different names.
The NIH sponsored The International Committee on the Nomenclature of Blood Clotting Factors. The committee held its first meeting in Rome in 1958. That is when the committee members made the decision to assign a Roman numeral to each of the clotting factors. At these meetings, the discoverers of ‘new’ factors presented their data, and the committee assessed the evidence. A vote was taken on the validity of a claim and an approved factor was assigned a Roman numeral.1
Around this same time, there was a patient being studied thought to have a condition known as ‘hypoproconvertinemia’ or SPCA by researchers at the University of North Carolina Chapel Hill. The researchers were Drs. Graham, Barrow, and Hougie, and the patient was Mr. Rufus Stuart. Convinced that this was a genetically recessive disease the researchers went to Stuart’s hometown in a rural mountainous region in 1955 and collected blood from his family members.
Lo and behold it turns out that Stuart’s parents were aunt and nephew which was important in isolating the blood clotting factor named after the patient. This helped prove that the mutant gene was autosomal and not completely recessive.
It was at the International Committee in Montreux in 1959 that the data on Stuart Factor was presented and accepted as its own unique factor. It was Dr. Leandro Tocantins of Jefferson Medical College in Philadelphia that gave an impassioned speech in favor of the designation as Factor X, Roman numeral 10.
Signs and Symptoms of Factor X Deficiency
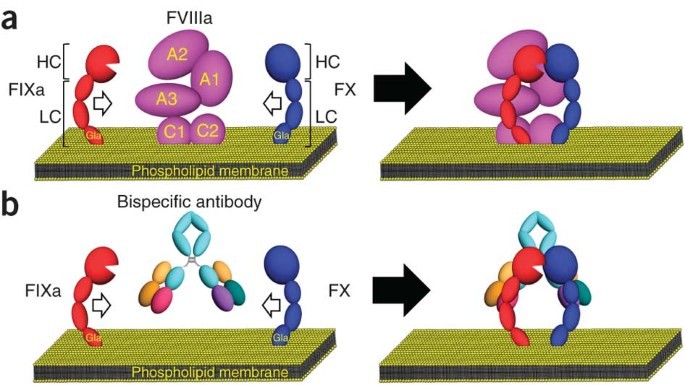
Factor X, which is produced (synthesized) in the liver, eventually interacts with other clotting factors and certain cells or substances, e.g., platelets or fibrinogen, to help to form a clot. Factor X deficiency is caused by a variation (mutation) in the F10 gene.2
The signs and symptoms of factor X deficiency are highly variable; this means that how the disorder affects one person can be very different from how it affects another person. Symptoms can develop at any age. Generally, the more severe the disorder, the earlier the symptoms begin.
Sometimes, factor X deficiency is broken down based on the residual amount of factor X activity. Individuals with about 40% or more protein activity have a mild disorder and often do not have symptoms (asymptomatic). Individuals with 10%-40% activity have a moderate disease and general symptoms associated with bleeding disorders. Individuals with 10% or less factor X activity have severe disease, particularly those with less than 1% of factor X. In some instances, the amount of secreted factor X is normal or near normal, but cannot function normally; in other cases, FX is not secreted at all.
Common symptoms of moderate and severe forms can include bruising easily, nosebleeds, and bleeding from the mouth and the gums. There may be blood in the urine (hematuria). Affected individuals are at risk of excessive bleeding during or after trauma or surgery. Some individuals may not have any symptoms except when they experience trauma or surgery. Without treatment, these symptoms can occur throughout life.
Women with factor X deficiency may experience heavy menstrual bleeding (menorrhagia). Pregnant women are at a greater risk of complications with their pregnancies including miscarriage or heavy bleeding during birth. Some women can experience heavy bleeding in the time after delivery (postpartum hemorrhaging).
Diagnosis
A diagnosis of factor X deficiency is based upon the identification of characteristic symptoms, a detailed patient and family history, a thorough clinical evaluation, and a variety of specialized tests.
Clinical Testing and Workup
Specialized tests will include screening coagulation tests that measure how long it takes the blood to clot, specifically two tests known as activated partial thromboplastin time (aPTT) and prothrombin time (PT). Individuals with factor X deficiency have both prolonged aPTT and PT.
Further tests, known as assays, are required to confirm a diagnosis and differentiate factor X deficiency from deficiencies in other clotting factors. An assay is a test that can measure the activity of certain substances in the blood. In affected individuals, a factor X assay will demonstrate the reduced activity of factor X.
Factor X can be detected using antibodies that have been generated to specifically recognize different forms of Factor X. Here is a partial list of available antibodies used for detecting and studying Factor X:
- Anti-factor X/Xa antibody (Clone GMA-529): GMA-529 (also known as α-HFX-27) binds human factor X and Xa in solid-phase ELISA and Western blot. GMA-529 prolonged FX-dependent clotting time, and activated partial thromboplastin time of normal plasma, and showed inhibition of thrombin generation.1 For the antibody to be effective, specific storage and handling instructions need to be followed. The antibodies should be distributed in small vials and aliquots stored at -20C if for a prolonged period. Repeated freezing and thawing should be avoided.
- Anti-factor X Heavy Chain antibody (Clone GMA-560): GMA-560 (also known as α-BFX-2b) binds bovine FX and factor Xa in solid-phase ELISA and Western blot. GMA-560 is partially calcium-dependent, inhibits FX activity in human, bovine, porcine, rabbit, and canine plasma inhibits the conversion of prothrombin to thrombin, and prevents inactivation of FXa by antithrombin III2. It can be used in the purification of factor X from plasma3,4 and blocks FXa-thrombomodulin interaction5. It is supplied in quantities of 0.1 mg and 0.5 mg and is unconjugated.
- Anti-factor X Light Chain antibody (Clone GMA-520): GMA-520 binds human factor X at an approximate molecular weight of 59 kD, under non-reduced conditions, and binds to human factor X light chain, at an approximate molecular weight of 16kD under reduced conditions. It can be paired with GMA-509 in sandwich ELISA assays. The Anti-factor X light chain antibody is only reactive to the human version of the protein.
Contact us: Contact Green Mountain Antibodies, the leading anti-factor antibodies producer, and learn more about our range of anti-Factor X at 802-865-6230
Sources:
- Stuart Factor: discovery and designation as factor X by J. B. Graham, First published: 25 April 2003 https://doi.org/10.1046/j.1538-7836.2003.00259.x
- Factor X Deficiency by Flora Peyvandi, MD., First published 2018 by National Organization for Rare Disorders (NORD) https://rarediseases.org/rare-diseases/factor-x-deficiency/